Wounded: ‘A small Scar will be much discerned’: treating facial wounds in early modern Britain
Article DOI: https://dx.doi.org/10.15180/191111
Abstract
This article examines the treatment of facial wounds in early modern Britain through a close study of the casebook of St Bartholomew’s Hospital surgeon Joseph Binns (d. 1664). It explores surgeons’ and related practitioners’ special attention to the care and infliction of facial wounds and scarring in their practice, including impairments to facial movement and expression, the use of specific suturing techniques and the reduced use of stitches, and the development of agglutinative medicaments. The face was recognised as a site of immense vulnerability and exposure, requiring particular care, and this vulnerability was mirrored in the capacity for facial scarring to detrimentally advertise a practitioner’s skill. This essay reads Binns’ unpublished notes against the cases and theoretical ideals set out in published texts from surgeons such as the Scottish Alexander Read, the East India Company surgeon John Woodall, and the London surgeon and physician Daniel Turner. I argue that both the textbooks and Binns’ practice demonstrate awareness of the special role of the face in the early modern period, and that this guided the medical approach to disfiguring injuries and conditions.
Keywords
Britain, disfigurement, early modern, face, Joseph Binns, surgery, wounds
Introduction
https://dx.doi.org/10.15180/Introducing his memoir of maxillofacial surgery today, Consultant Surgeon Professor Jim McCaul highlights the special pressure he feels operating on the most visible site of the body:
All surgeons carry out procedures that enhance their patients’ lives and are often life-saving, but maxillofacial surgery carries an additional burden of significance and responsibility. A livid breastbone-to-navel scar left after open heart surgery might be a little unsightly but it will usually be covered by a patient’s clothes, and even when exposed on a Mediterranean holiday it is not a repugnant or frightening sight. Similarly the scar left on a woman’s abdomen by a Caesarean section will be concealed by her everyday clothes or hidden by her bikini at the beach and will have no impact on people’s perceptions of her. However, because our identity is so closely tied up with the face that we present to the world, facial scarring, whether it is caused by trauma or disease, or the surgery to cure them, has an immediate and potentially profound impact on our relations with those around us.
Such concerns have led to the development of specific techniques and principles that privilege not only function but also aesthetics in facial surgery in ways that exceed equivalent concerns for less visible parts of the body. McCaul’s implicit suggestion that equivalent ‘livid’ scarring of the face can be perceived as ‘a repugnant or frightening sight’ that will have an ‘impact on people’s perceptions of [the individual]’ is to some extent supported by contemporary studies on the stigmatisation of individuals with significant facial differences, while being increasingly nuanced and even challenged by studies on disfigurement in different historical contexts.[1] Surgeries and products to ‘fix’ non-normative faces comprise a controversial and highly lucrative industry, while disability activists critique any obligation toward ‘normalising’ surgeries, with the UK disfigurement advocacy group Changing Faces calling for education and ‘face equality’ that embraces and respects variation (‘About Face Equality’). Most recently, the transplantation of all or parts of faces has become both a reality and a highly contentious issue, raising questions of identity, risk and even the ethical question of replacing what might be a solely visible difference of the face with the serious physionomical implications of immunosuppression reliance (e.g. Perpichj, 2010).
Early modern surgeons and related practitioners also acknowledged a special onus upon their skills when treating facial wounds and other disfiguring conditions. Barber surgeons treated people across the social spectrum and offered a variety of services to maintain a neat and healthy appearance of the body and face (Pelling, 1986). The face was seen as vulnerable both because it was uncovered, and because it was thought to be a softer, weaker section of the body more liable to wounds and diseases (Skuse, 2015, p 26). The face also carried deeper associations of honour and identity, with severe disfigurements even carrying dehumanising associations (Skinner, 2017, pp 41–66; Groebner, 2004; Delaporte, 2013; Agamben, 2000). This vulnerability was mirrored in the capacity of the face to advertise a medical practitioner’s skill, or lack thereof. Surgeons and physicians therefore paid special attention to the care, and infliction, of facial wounds in their practice. They utilised specific suturing techniques, covers and agglutinative medicaments, and while the first priority for head wounds was always to prevent death, further interventions were predicated on arresting disfigurements, and not causing excessive scarring or impairing facial movement and expression.
This article will use theoretical ideals set out in published medical texts to examine the treatment of facial wounds in the 1633–1663 casebook of Joseph Binns (Sloane MS 153), who was surgeon to St Bartholomew’s Hospital. The majority of the cases discussed here are responses to disease or trauma and are particularly useful as evidence because of the age and gender spread of patients. Both the textbooks and Binns’ practice demonstrate awareness of the special status of the face and facilitate the extrapolation of key principles for surgeons approaching facial wounds in the early modern period. The face has been largely overlooked in histories of pre-modern disability that focus on people who were rendered physically incapable of labour, but studies are increasingly unearthing the experiences of people living with severe disfigurements in different historical periods. More evidence is emerging of people whose facial appearances affected their ability to work and support themselves, get married, or otherwise fully engage with their communities and social roles, such as a seventeenth-century man whose face is severely disfigured with a canker describing himself in a petition for relief as so ‘loathsome’ that ‘no one will imploy him’.[2] This growing appreciation for the importance of facial appearance and health therefore necessitates more specific work on medical care available for disfiguring conditions.
Part of this enquiry must concern the extent to which people with disfigurements were considered, or considered themselves to be, disabled. The latter of course presents a significant problem of evidence. Medical and legal accounts are more interested in the infliction or treatment of a facial wound than with the effect of it on the individual’s social capital or sense of identity. This article suggests that unpublished sources such as Binns’ notes, though sparse, can provide useful material. Although they are in no way an unmediated text, they get closer to Binns’ daily practice, and are more likely than published medical treatises to include cases of failure or hesitation that don’t fit into the narratives of knowledge and authority promoted by published accounts more invested in the self-fashioning of their authors.[3] Here and in some published accounts we also catch glimpses of people living with facial differences, either in direct references to their delaying treatment or rejecting further interventions, or in the chatty asides still characteristic of some medical treatises.
Joseph Binns in context
https://dx.doi.org/10.15180/191111/002Joseph Binns (d. 1664) was born in Derbyshire and served as apprentice to London surgeon Joseph Fenton before travelling as a surgeon with the Parliamentary army during the Civil Wars. From 1647 to 1664 he worked as one of the surgeons at St Bartholomew’s Hospital, and the casebook includes over 600 of these patients (Beier, 1988, pp 51–52). Lucinda McCray Beier (1988 and 1992) has offered the most extensive examination of this source, reading Binns’ casebook for evidence of day-to-day practice and as a comparison to the published work of surgeons such as Charles II’s sergeant surgeon, Richard Wiseman, for evidence of distinctions between theory and practice. Her final assessment is that Binns was ‘cautious and very conventional’ in his practice (1992, p 96). Lauren Kassell points to Binns’ manuscripts as an exception to the prevalence of casebooks from surgeons who ‘fashioned themselves as physicians’, finding him instead to demonstrate ‘little evident scholarly imperative’ in his notes (2014, p 617). This pragmatic and decidedly surgical focus makes Binns a useful testing point for everyday surgical approaches to facial wounds in London during this time.
The research presented here focuses on Binns’ approach to facial wounds in dialogue with published tracts. It supports Beier’s general assessment of Binns’ conservatism by demonstrating, for example, that Binns resisted intervention in aesthetic cases that did not also involve pain or risk of further complications. This contrasts with evidence from more ambitious figures like London surgeon and physician Daniel Turner (1667–1741) who were willing to remove non-painful marks and growths (Cock, 2017). Officially, external treatment was the purview of the surgeon, while only physicians could administer internal medications, but in practice these lines were often blurred, and Binns frequently prescribed laxatives and emetics (Beier, 1992, p 81). He also records consultation or engagement with a number of surgeons and physicians, including John Woodall (1570–1643), who had also worked at St Bartholomew’s. Woodall had extensive experience in army medicine before he was appointed the first surgeon-general of the East India Company in 1613 and he became well known for naval surgery after the publication of his guide to the field, The Surgions Mate (1617 and expanded in two subsequent editions) (Crawford, 1914, pp 19–20).
Binns’ casebook offers an additional resource to the medical history of the British Civil Wars by demonstrating forms of medical care available in the affiliated hospitals. There is increasingly exciting scholarship about the medical provisions available in this conflict, including specific attention to facial wounds in this and previous eras in which the face was the most exposed part of the soldier’s body (Appleby and Hopper, 2018; Gruber von Arni, 2001; Tracy and DeVries, 2015). For example, in 2016 the new National Civil War Centre in Newark (Nottinghamshire) hosted an exhibition devoted to medical provisions available during the conflict, and prominently featured an imagined portrait of Parliamentarian Colonel William Forbes, who lost an eye and a significant amount of facial skin and muscle from the wind of a cannonball at the siege of Pontefract in January 1645, after which he was known as ‘Blowface’.[4] Scholarship on facial surgery in and following the First World War, including its broader cultural and psychosocial implications, is perhaps leading this field at present, having formed a significant thread of academic and public scholarship around the recent centenary.[5] While early modern discourses foregrounded the honour that could accompany the ‘Hacks and Scars, those rugged Beauty Spots of War, which [men] wore as true marks of their undaunted Bravery’ this potential was never uncontested, and cases like Forbes’ highlight the capacity for public insults, disabling discomfort and rejection that could accompany more substantial changes to the face (Ward, 1700, sig. ix.O3v).[6]
People with significant facial differences were regularly encountered in early modern Britain, and their appearance was commented upon. Samuel Pepys (1633–1703), who suffered his own eye troubles, records numerous men with one eye: ship’s mate, Richard Cooper, for example, who teaches him mathematics; parliamentarian soldier John Hewson (d. 1662); a ‘Frenchman with one eye’ with whom he hails a coach (31/12/60); and the calligrapher Richard Hoare. Further mentions of people with visible eye issues include ‘the faire Mrs. Margaret Wight’ for whom ‘the cast of her eye, got only by an ill habit, do [sic] her much wrong’ (1/06/66); James, Duke of York, who wore patches after being struck in the face by a branch while hunting; the sailor John Daniel whose eye is temporarily ‘stopped with okum’ to cover a battle injury (4/06/66); and even the black eye Pepys himself inflicted on his wife, Elizabeth, on 19 December 1664 (Pepys, 1970–1983). There is also ample evidence in contemporary accounts of surgeons’ and physicians’ attempts to minimise such facial differences: Daniel Turner records the case of a boy who pierces his eye while sewing a football. When the boy’s eye could not be saved he was fitted with a glass one by a Mr Boyce that was such a close match to his natural eye that neighbours ‘could not distinguish the one from the other’ (Turner, 1722, Vol 1, sig. Bb2). Prevalent diseases like smallpox and the pox (syphilis) caused characteristic disfigurements (which Binns treats with some frequency), while astringent medicaments used to treat these and other disorders could themselves cause further damage to the skin. Serious burns to the face appear frequently in surgical texts, and accidents, fights and deliberate attacks were further sources of facial injuries and scars. Wendy D Churchill’s survey of many of these cases suggests that men were more subject to serious injuries and violence that might take them to the surgeon, while women might treat minor scalds and other injuries at home (2016, pp 50–54).
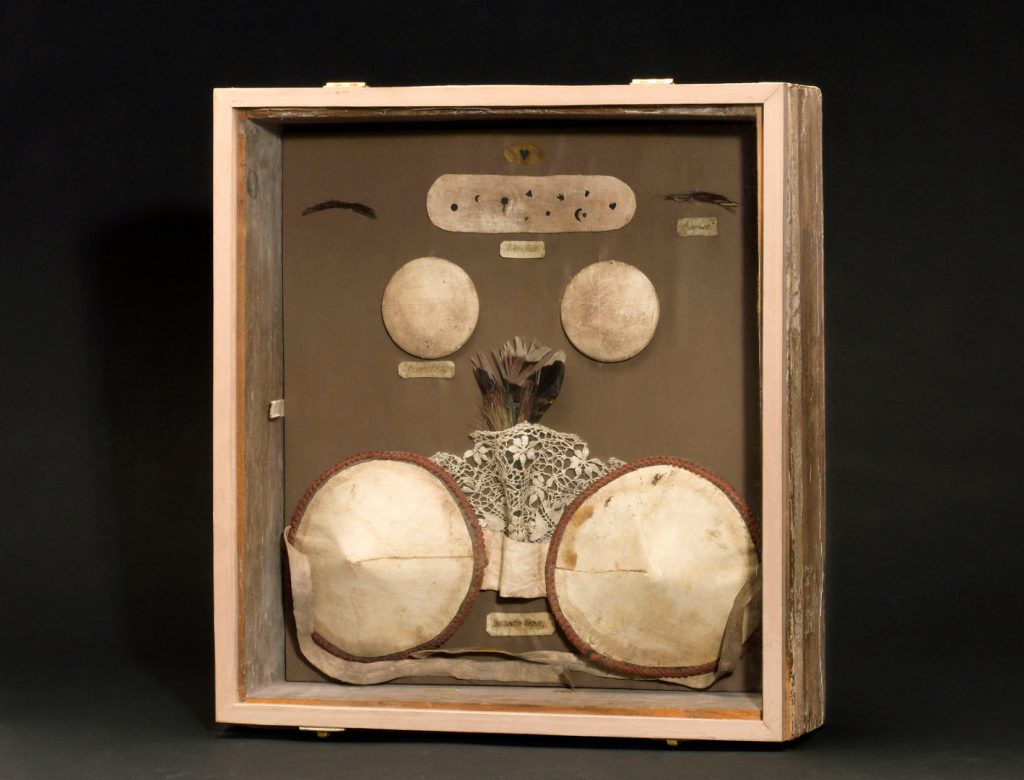
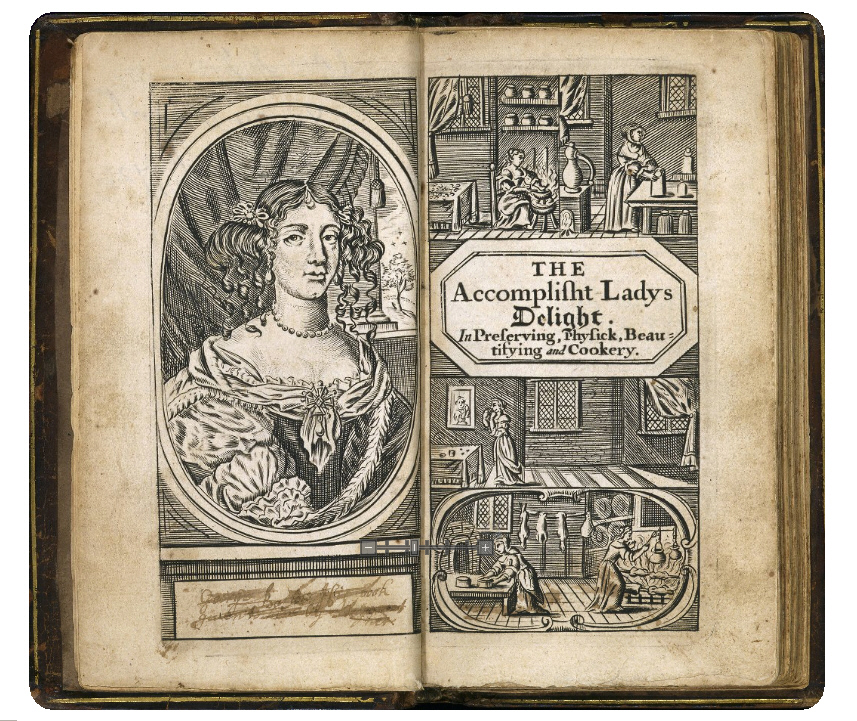
Early modern medical manuals for home and trade were full to bursting with ointments, washes and other concoctions to clear the skin, teeth and hair, and combat minor ailments that would have included aesthetic components, while the market was full of powders, patches, plumpers and pastes that could cover blemishes or fill in pockmarks or scars (Leong, 2008; Stobart, 2016; Jenner and Wallis, 2007).

Volumes like Hannah Woolley’s The Accomplish’d Lady’s Delight in Preserving, Physick, Beautifying, and Cookery (London: B Harris, 1675) contained numerous recipes for the face and body alongside domestic food preparation, for example. There was therefore no shortage of work for practitioners who could offer special skills in treating facial wounds and conditions.
Living with facial differences: delaying treatment
https://dx.doi.org/10.15180/191111/003Medical case notes, especially those as brief as Binns’, are not ideal for capturing the experiences and views of the individuals whom he treats. Yet these sources can serve as evidence for people living with facial difference, especially where they describe individuals who have significantly delayed seeking medical intervention. Some of these people might have sought other forms of healthcare: facial swellings might have been treated with domestic medicaments, for example, or people may have hoped that they would ease of themselves in order to avoid the expense, pain and variable success rates of surgeons and physicians. Elizabeth Pepys applied a poultice including butter and parsley to her bruised eye but sought a surgeon’s assistance for an abscess in her cheek that the surgeon warned ‘may spoil her face if not timely cured’ (discussed in Weisser 2009, pp 326–7). Binns’ delayed cases involve both men and women and suggest that many people lived with aesthetic conditions until they caused pain or impeded facial functions. In 1661, Binns records seeing a ‘Mrs Avery of Whitchurch neare to Redinge, [who] had a fall some yeeres since & cut her upper lippe on ye underside the stringe in sunder & drive in one of her upper teeth in to the gumme against the stringe’.[7] We don’t know what treatment she sought at the time of the accident, or whether there was significant visible injury. Her visit to Binns is prompted not by a ‘tooth… [that] tuned Blacke 8 or 9 weekes since’, but by an apostem (abscess) in her upper lip that has now expanded to the nose and created a passage from the mouth to the nasal cavity, which he assumes is ultimately linked to the earlier fall.[8] In other words, although the two are related, it is the functional impairment to swallowing that prompts Mrs Avery to visit, rather than concern about the black tooth. Binns’ cousin’s wife has a rotten tooth and swelling from May 1654, and seeks treatment from him in July including incision to drain it on the 23rd, after which she interrupts her treatment for a journey to Wales. It is described as ‘all most well’ upon her return in September, but after more swelling and weeping the tooth is drawn on October 2, ‘soe it siccatrised [cicatrised; started to heal to a scar] in 4 dayes aft’ (f. 130r–v). Other cases show that the discomfort and visible difference could be intermittent, such as ‘ye Lorde ffairfaxs man’ who has a tumour under his tonge and ‘a little tumor outwardly’ who was ‘troubled with it once in 3 or 4 years’, before it suddenly ‘cracked’ and released a stone like a date pit (f. 7v).
Binns’ scrofula cases show similar delays in the patient seeking treatment until a visual condition has become painful. We are told that Miss Elizabeth Oldbury had been ‘troubled wth scropulous tumers on her necke on both sides this 2 or 3 yeares’ yet she seems only to have sought out Binns’ help because for the last three months the left side had begun to swell, grow red and sore, and develop into an abscess. Binns records ‘open[ing] it wth the causticke the 12th Januarie’ (the caustic stone, a solidified, highly alkali mix of quicklime and potash, was a favourite of his remedies) and that it is ‘well’ in three weeks (f. 68v). Mrs Hancocke similarly lives with a painless ‘little wenne or a scrophulous little tumor as bigg as a large Nuttmeg’ on her neck ‘for a longe time’, and only seeks out assistance in 1661 when ‘it began to be red & payneful & swelled much & in ye begininge of march there was Matter in the toppe of it’. Binns opens it with a lancet and uses drying medications, recording that ‘soe it was consumed, & well the 25 Marche’ (f. 93r). Binns provides another detailed treatment account for Mrs Elisabeth Barker’s ‘Scrophulous Tumors in the Necke’ between 1655 and 1659 (ff. 78r–79r). He tries a number of approaches, including frequent laxatives, and records their occasionally disfiguring symptoms, such as one that ‘caused severall pimples & to ulcerate & runne’. Perhaps after four years Mrs Barker saw insufficient progress in her case to bear further with Binns’ regime, as the final note – with a hint of pique from Binns – is a curt record that ‘She was after Touched by ye Kinge’ (scrofula being the ‘King’s Evil’ and supposedly cured by the Royal Touch) (f. 79r).[9] Thus, individuals with disfiguring conditions might not seek out treatment immediately, but as with all health care they had access to a wide range of regimes, among which the surgeons were just one option. It was trauma in which the latter held the lion’s share of the market and which forms the focus of surgical treatises on aesthetic principles as discussed below.
Facial surgery and trauma
https://dx.doi.org/10.15180/191111/004The evidence shows that surgeons were willing and able to perform significant incursions upon the face but that they also recognised the special requirements of such procedures. Practitioners developed a range of techniques and principles for treating head and face wounds that would in the first instance prevent death, but that would also prevent, arrest or even rectify disfigurements. These built on classical and medieval surgical traditions, and were passed on to apprentice surgeons through practical experience, professional treatises and semi-weekly lectures at the Barber-Surgeons’ Hall.[10] One of these lecturers was pragmatic Scottish-born surgeon and physician Alexander Read (c. 1580–1641), who trained in Aberdeen and Europe before practicing in Scotland, Wales and London. Read emphasised the special status of the face as ‘the seat of comeliness and beautie’ and the vital marker of individual identity (Read, 1638, sig. Aa1r). The surgeon must therefore ‘have a speciall care that you leave no foule cicatrix (scar) after the curation of the wounds of it, if you be called to cure them’ (sig. Aa1r–v). Read gives particular instructions for treating wounds to ‘prevent ill favoured scarres’, the first of which was avoiding stitches wherever possible. If stitches were necessary, he writes, they should be administered with as small needles as possible, using thin stitches of waxed flax that wouldn’t cut the skin, and should be removed as soon as it was safe to do so (see below for a detailed discussion of stitching). The surgeon should then avoid any drying powders that will hinder regrowth or constrict the new skin (sig. Aa1v–2r). Binns adopts several of these techniques in his practice.
While surgeons like Read stressed the means by which they could and should reduce the level of scarring, there was a resignation about the limits of surgical intervention in the face. As Hannah Newton has recently demonstrated, early modern medicine incorporated ample consideration of recuperation and recovery – when considering ideas of illness, health might even be understood as not simply an absence of pain or disease, but as the active sense of strength, the ability to return to everyday life, or ‘feeling completely better’ (2018, p 231). Binns and other surgeons’ case notes, however, suggest that treating a facial wound to the stage of cicatrisation was an accepted point at which the surgeon’s job was satisfied. For example, the 1720s notebook of Bristol apprentice surgeon Alexander Morgan records a case in which a young man had been fighting and received a deep wound on his forehead. Morgan cleaned and redressed it every day for eight days, at which point it cicatrised and the man was considered ‘cured’ (in Fissell, 1991, pp 53–54). Binns likewise regularly finishes his case notes at the point of cicatrisation, or even before. In one case he records that on ‘The 22 August Mrs Sheepewashe her sonne was wounded upone the eye browe ye lefte by a horses heele the wounde triangula ye eye browe torne upe’. Binns records another surgeon closing the lips of the wound and binding them with a pledget (wad of lint, cotton or related soft material) and plaster. It is opened again the next day, and reveals ‘much bloodye moysture’, whereupon Binns wraps it up again with an additional poultice, applying further dressings on the 26th and 29th. At this latter date, Binns records that ‘noe digestion comes from it [that is, pus as a sign of the wound maturing] but bloody moysture allmost closed, well’, suggesting that in the absence of complications in this case he considered his task concluded and the patient ‘well’ at the point that the wound showed signs of healing cleanly, but long before the point of cicatrisation (f. 104r). Treating a coachman’s wife in 1636 for a rapidly growing tumour in her cheek, Binns closes the treatment of several weeks with ‘all ye sores dried up, & the Tumor less than it used to be praysed be god’ (f. 155v). In this case, closure of the wound and reduction (not absence) of swelling was sufficient for her to be dismissed. Beier reads Binns’ definition of ‘well’ as ‘limited at best…. His was no miracle surgery which could restore lost beauty or promise permanent cures’, suggesting that he aimed rather for ‘stability’ (1988, pp 86–87). There is every possibility that these patients sought further care from other practitioners, practised home care, or used cosmetic products (such as the many recipes for ointments to reduce scarring), but for Binns his responsibility closed with the wound.[11]
This aim of ‘stability’ included the prevention of further visible effects, and a heightened concern to reduce scarring was a key difference between surgery for the face and the rest of the body, even as it accompanied familiar protocols for arresting the growth of tumours and infections on the covered body. In addition to attending to the wound as it presented, it was important for the surgeon to prevent the progress of small blemishes to bigger injuries, such as the movement of smallpox pits to gangrene if septic matter was allowed to develop, or indeed was introduced by other practitioners. In September 1646 Binns treats a button-maker’s child who has recently recovered from the smallpox, but whose pocks on her palate have developed into a ‘putrefactius ulcer’, with corrosion and loosening teeth. Binns provides an unspecified gargle and cordial, but records that her face begins to swell, and a black spot appears near her left nostril. This blackness continues to spread, ‘soe that in 3 dayes more [after 8th October] it toke all the upper lippe & for a rounde compass one bothe cheeks to the tipp of the nose’ (f. 12r). In this case, risk of further disfigurement was disregarded as the child weakened, and subsequently died on October 12 but the initial concern to prevent escalation of the visible injury is clear. Binns is frequently called upon to assist in cases originally ascribed to tooth problems, sometimes after a drawing of the tooth by someone else has failed to arrest further infection. For example, Mr Dakins, sees him after receiving dental work from ‘the barbar at holborne bridge’ (f. 175r). In his surgical textbook, Woodall highlights the need for timely and skilled drawing of teeth, from the lack of which ‘sometimes proceedeth great swellings in the face, or in the amygdals [tonsils] and throat, and the party is suffocated and dyeth: Likewise by indiscreet drawing of a tooth, either the jaw is broken, or some other bad accident is provoked’ (1655, sig. E2v). In detailing tools for the operation, Woodall draws on his own experiences as both a surgeon and a patient, attesting that hard steel instruments are the best, as ‘My self have (to my pain) proved experience in my own head twice’ (sig. E3r). Woodall’s interest was particularly relevant for his sea surgeon audience, since tooth loss was a common result of scurvy.
A major source of facial trauma for Binns’ patients was the civil wars, since St Bartholomew’s Hospital received a significant percentage of military wounded. Several fatal head wounds appear in Binns’ notes, such as Christopher Wallye, a royalist trooper under the command of Lord Willoughby d’Eresby, who was shot at the Battle of Edgehill (23 October 1642) (f. 188r). In other cases, soldiers receive treatment for survivable wounds. On 5 July 1642 Binns treats ‘The Lorde Morlyes man’ for a cut ‘beginninge at ye upper parte of the lefte side of the os frontis [forehead part of the skull] nere the temporal musclle through the midle of ye eyebrowe, & soe in a direct line across the nose through ye cartilage of the nose, & soe quite through ye right nostril’. This was probably a royalist soldier under the command of Sir John Morley, and sounds like a slash from a right-handed swordsman, but Binns only describes him receiving the wound ‘at nighte’. Despite what sounds like a very serious wound, Binns records that he only inserts one stitch in each of the nose and forehead, ‘the reste wth slippes of plaster’ and balsam (f. 193v). The use of minimal stitching and plasters for facial wounds was a recognised means of reducing visible scarring, and it is notable that this detail was retained even during conflict.
Stitches and scarring in facial surgery
https://dx.doi.org/10.15180/191111/005Surgeons were encouraged to take particular care with all wounds requiring stitches in order to minimise their visual impact. Even Woodall, speaking to surgeons who would probably be attending to men in battle, on ships, or in other less-than-ideal conditions, exhorted them to, ‘when you stitch, beware you draw not the orifice awry, oblique or deformed, but that you have great respect to the true beauty and former comlinesse of the wounded part, neither let your stitches be too near unto another, neither tie your silk too close, which will occasion the stitches to break before their time’ (sig. F2v). Surgeons developed particular techniques for suturing the face, designed to minimise scarring by avoiding needle perforation of the skin itself. One of the most recognisable was the ‘dry seam’ or ‘dry suture’. This involved the use of patches of linen that were stuck to the skin and then stitched together to draw the lips of the wound close and achieve adhesion, rather than stitching into the skin itself. This technique could also be used in conjunction with mixtures, often based on egg whites, that glued the lips of wounds closer together, and in minor cuts might remove the need for stitching altogether. Woodall promotes the efficacy of the dry suturing technique for avoiding scarring when combined with ‘a sure natural balm’ but declines to explain it in his book on the grounds that it is impractical to perform at sea (sig. P3v). His reticence highlights one of the many external factors that might affect not only the occurrence of particular injuries themselves, but also the treatment received and the level of facial disfigurement incurred: from patients’ employment, gender, status, to the geographic locations of injury and treatment.
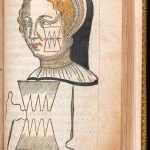
The importance of the dry stitch is emphasised by its frequent illustration in contemporary texts.

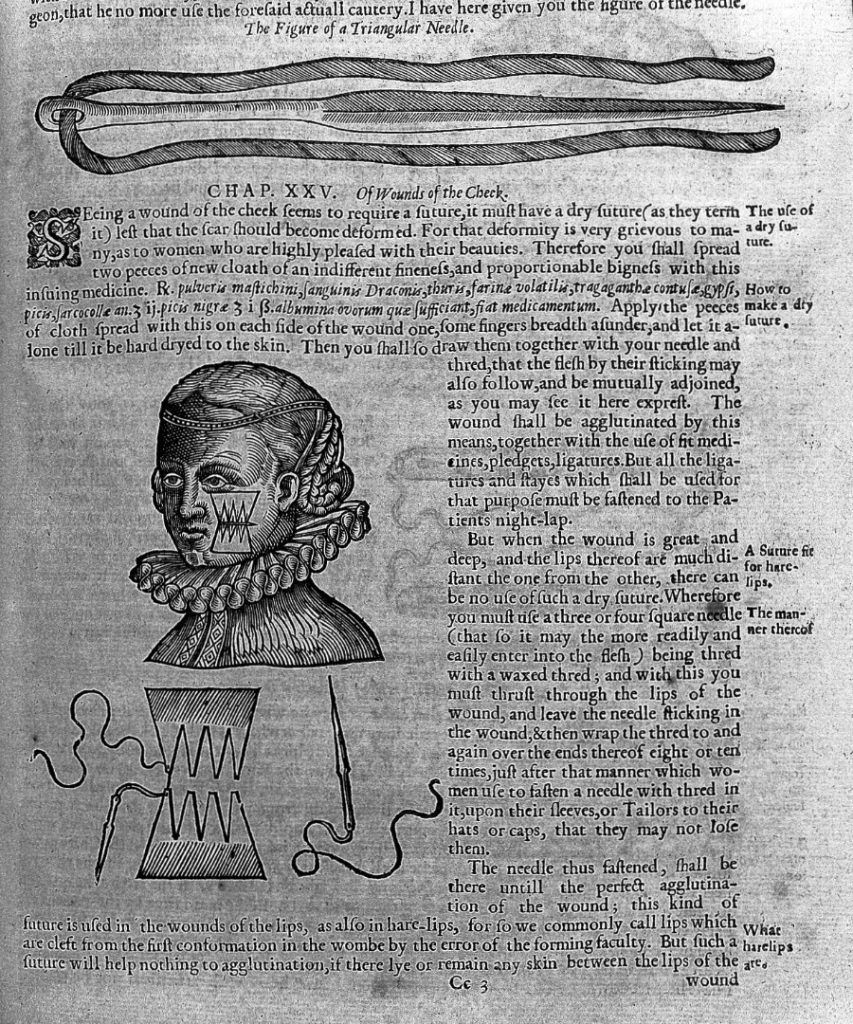
One often-repeated image first appeared in Ambroise Paré’s (c. 1510–1590) La methode curative des playes, et fractures de la teste humaine (Paris: 1561). It depicted a neatly dressed woman with a completed dry seam on her cheek, alongside an illustration of the plasters and needles in media res, the whole clearly showing that the patches rather than skin were being stitched together. The image was often adapted in later publications by giving the woman current and more local clothing, thus ensuring that the technique appeared up-to-date. One variation appeared in the French and English editions of Jacques Guillemeau’s (c. 1550–1613) Les oeuvres de chirurgie (Guillemeau, 1598, p 143; 1598b, sig. b1r). Peter Lowe (1550–1612), who practiced briefly in London before settling in Glasgow, copied Guillemeau’s illustration for the extended 1612 edition of his Chyrurgerie (1597) (1612, p 288). The image was anglicised with a modern outfit for the woman for Johnson’s 1634 English translation of Paré’s complete works, and this version was retained for the 1665 edition. Johnson’s printer, Thomas Coates, used this version in Alexander Read’s extended summary of Helkiah Crooke’s Microcosmographia (1615), published as Somatographia anthropine (Read and Crooke, 1634, sig. Z3r).
There is a particularly strong gendering of the operation at work in these illustrations of the dry seam, and in contemporary comments on the process, although this is less evident in Binns’ case notes. Not only is the illustration a female patient, but additional comments tied the operation to the desires of women to minimise facial difference. Surgeons stress both theoretical and practical reasons for taking additional care with women’s faces: not only do they protest that it is the female patients who insist on minimising scarring, but also that male patients will have the advantage of hiding behind honourable disguises such as beards.[12] Paré describes the additional care for cheek wounds to prevent scarring as important ‘principalement les belles dameoiselles’ (‘especially to beautiful women’), which entered Johnson’s edition as a slightly broader remark that the ‘deformity is very grievous to many, as to women who are highly pleased with their beauties’ (Paré, 1561, sigs. Hh8r [text], and Ii1r [illustration]; Paré, 1634, sigs. K5v, K6r [illustration]). Thus Read stresses the need to take additional care to ‘avoyd scares which will make the face deformed. For that is the market place, especially in women, to please whom Chirurgians have devised this kinde of Suture’ (Read and Crooke, 1634, sigs. Z2v–Z3r). The face as the ‘market place’ of the body was a proverbial phrase that extended to both men and women to emphasise the importance of the face as a site of sociability and community, and that of facial appearance for an individual’s economic success.
Despite such protests, Binns employs plasters and the dry seam with male and female patients. His delayed scrofula patients may also serve to query surgeons’ insistence that women were likely to seek pressing responses to aesthetic grievances. On 14 February 1639, Binns opens a large tumour on the nose of Mr Edward Talbott to remove the ‘core’, then in lieu of stitches treats him ‘wth an incarnative powder & slippes of plaster then a peece of white sparadrap [i.e. linen or other bandage] to bringe the jagged edges smoothe’ (f. 175r). Similarly, a child named Joseph who falls and cuts across the corner of his mouth on a stair is first given two stitches, before they are replaced with ‘slippes of plaster’ after four days (recall here that Read had advised replacing any unavoidable stitches as soon as possible) (f. 219v). Reducing stitches was therefore a widely applied principle.
Recognising the aggravating potential of stitches, surgeons employed topical and agglutinative medicaments to close the wounds wherever possible. This included the use of drying medications for sores, rather than cutting them out. When called upon to treat a nine-month-old baby who has been moderately torn across the cheek by a dog bite, Binns administers a plaster dipped in spirit of wine to the child’s face, and gives the mother Theriaca Londinensis (‘London Treacle’) made of hartshorn (deer antler, a source of ammonia) and marigold medications to pass on its strengthening qualities through her breastmilk (f. 188r).[13] Not all of the surgeon’s tools detailed by Woodall are for cutting, but instead include things like the ‘speculum oris’, which was specifically designed to clamp the tongue and chin, ‘very necessary to hold open the mouth for better applying medicines to the throat’ or to administer liquid food (Woodall, 1655, sig. D4r). As Beier notes (1988, p 84), Binns privileges interventions that don’t include the knife: he performs very few amputations, instead showing preference for treatments like poultices, the caustic stone, and other external interventions, along with laxatives and emetics.
In addition to taking care with stitching, there is some evidence that, when cuts were required, surgeons might attempt to do so on less visible parts of the body. Turner approvingly cites James I’s physician, Sir Theodore Turquet de Mayerne’s regimen for a facial redness, which included cupping the nape of the neck, scarifying between the shoulder blades, placing ‘Leeches behind the Ears and on the Inside of the Nostrils’, and opening ‘the Veins of the Tongue’ (1714, sig. N1r; added emphasis). Binns similarly treats a woman who has been troubled by ‘Anchylops’ (abscesses in the inner corners of the eye) for four or five years – now developed to further symptoms, such as sloughs from the nose – between her shoulders, after other surgeons have done so on her neck and arm (f. 37r).
Preserving the sense organs and facial mobility
https://dx.doi.org/10.15180/191111/006Surgeons were very aware that the face was also different from other areas of skin for including a variety of natural openings and organs of the senses. The eyes, for example, could be easily damaged, and any ointments applied near them should be thick enough not run into them. Turner talks about making a linen mask that can be lined with the relevant ointment (thickened with wax) and laid on the face, so as to keep it in place and undisturbed (1714, sig. S6v). In other cases, a feather could be dipped in the mixture for gentle application, which is how Binns administers a balsam to the face of a barber’s child after s/he is ‘shot in ye face wth ye cornet of gunpowder’ (f. 187r). Turner records a couple of incidents in which men have sections of an ear bitten off in a brawl: either because the piece is eaten, or too ‘mangled and unequally torn by the Bite, and trampled under Feet in the Scuffle’, the ears in these cases cannot be reattached. We do learn a little more about one of these men and his reconciliation with his disfigurement: being ‘of a frolicksome and forgiving Temper’ he reconciles with his opponent, and keeps the section of ear at home, ‘to look upon in a Bottle of Spirits’. We are then told that he has a running gag with people in which he agrees to a set price for ‘some particular Sort of Goods as would only reach from one of his Ears to the other’, before revealing the true distance in his case (1714, sig. U1r). While the ears were not considered vital for hearing, they played an important visual role that was exacerbated by the use of ear-cropping as a punishment. All senses (but most importantly eyesight) were considered important for full engagement with the community and wider world (Porter and Bynum, 1993; Cockayne, 2003; Milner, 2011).
Other medical techniques responded to the face’s need for movement for functions like eating, speech and emotional expression, including the capacity for surgical interventions in the face to actually cause significant damage to muscles and nerves. Physician John Bulwer (1606–1656) wrote a number of texts concerned with the body’s capacity for non-verbal communication. In Pathomyotomia or a Dissection of the Significative Muscles of the Affections of the Minde (1649), he wrote that if a man’s facial musculature was immobilised, ‘all the inward motions and affections of his mind would be obscur’d in silence, and become altogether invisible’ (sig. C8r). It appears to have been well known that surgeons could themselves cause this paralysis. Bulwer warns that the muscles above the eyebrows (a feature he sees as particularly expressive) serve to ‘deteine the Eye-brows in their native posture and situation; whose use of what decency and importance it is, appeares in those who by the unskilfulnesse of Chirurgions, and a transverse Dissection of the fibres of these Muscles, have been deprived of the use of these significations of the Mind’ (1649, sig. H3v). He reiterates this warning later in the book, and cites an additional ‘example of a Cardinall who having the left Muscle cramped with a wound, could not move the one halfe of his Forehead’ (sig. G12v). Similar remarks of ‘Caution for every young Chyrurgeon that he makes no transverse Incision here’ appear in John Browne’s A compleat treatise of the muscles as they appear in humane body (1681, p 11), and in William Salmon’s Ars chirurgica (1698), and ultimately echo the warnings of much older surgeons, such as Guy de Chauliac in Chirurgia magna (1363; 1997, Vol 1, book two, chapter two, p 35). Salmon states explicitly that “The Temporal Muscles are to be avoided,… Because a Paralysis will be caused on that side the Head, on which the Wound is made, and a Convulsion on the other side, by which an uncomely Distortion of the Face will be made’ (1698, p 1235. Original emphasis). A specific distortion raised by Bulwer is the ‘cynic spasm’, which he also refers to as a ‘plaise mouth’ (after the fish) or ‘dog spasm’, since ‘cynic’ derives from the Greek κυνικός, meaning dog-like. This could also be used interchangeably with tortura oris (contortion of the mouth). The disfigurement is characterised by the patient drawing his or her mouth to one side, with barred teeth, hence its association with an angry dog, or the side-mouthed fish. In Pathomyotomia, Bulwer warns that it can result from ‘Chirurgions in their incisions in these parts…by an over free cutting of the transverse fibres’ (1649, sigs. K6v–K7r). Browne, drawing ultimately on the Roman encyclopaedist Aulus Cornelius Celsus’ De Medicina (IV.3), also writes at length about the different muscle spasms and contractions judging that ‘there is no Disease more outrageous, cruell, and acute, than that which by a Rigor or Stiffness of the Nerves and Sinews does annex the Head to the Scapula’s, the Chin to the Breast, and maketh the Neck right and immovable’ (1678, sig. I2r). Physicians also offered internal remedies for tortura oris, with John Hall (1574/5–1635) treating his own daughter for it in 1623–1624 (Hall, 1657, sigs. C12r–D2r). Such frequent and specific mention of the issue demonstrates the recognised importance among surgeons of maintaining malleability of facial muscles in addition to smooth, unbroken surfaces when treating or creating wounds to the face.
Binns doesn’t record causing any such paralyses, but does provide cases of disrupted facial muscle movement. In June 1640 he records treating the son of Mr Webster from Chesterfield for ‘a wrie necke’ which he treats with a ‘waye of cuttinge’ recommended by Mr Harris (unidentified). He appears happy with the result that ‘it was skinned in 5 dayes’ (f. 176v). Here we again see the cessation of the surgeon’s involvement at the point of cicatrisation, which suggests that in this case there were no further problems of impeded movement. In some other cases, however, Binns alludes to the constriction of movement resulting from scar tissue. In 1634 Binns treats a maid, Elizabeth Bemis, who is ‘burned wth fyer upon the left Temple close to ye eye lid… almost to ye cranium’. Binns’ treatment includes opening a vein, a clyster, cupping, and applying a poultice ‘to remove ye escars’. Binns records satisfaction with the treatment, but as the area begins to scar it constricts the skin around Elizabeth’s eyelid, drawing it open painfully. She is ultimately relieved of the pain by bleeding and having the eyelid stroked by the hand of a dead – presumably executed – man (f. 151v).[14] In August 1649 Binns treats a ‘youth’ who can barely open his mouth on account of scar tissue after ulceration of the cheek and gums. Binns ‘divided it wth a knife’ and placed softening medicaments and a piece of lead in the mouth to keep ‘his jawes assunder but he would not suffer it soe as they contracted againe allmost as close as it was afore’ (f. 211r). The case is not resolved, suggesting that the young man may have continued to experience restricted mouth movement.
Spasms and other facial marks were also known to be possible outcomes for the pox. This was customarily treated with mercury to provoke sweating and spitting (salivation, or fluxing), which physicians and surgeons were well aware carried significant side effects. Physician John Cotta wrote that ‘some fall into consumptions and marasmes, some lose their teeth, some have the palate of their mouth rotted, some the very bones of the head eaten, some by convulsions their mouthes and faces set awry’ (1612, sig. B3v). Binns records treating over 130 people for pox or gonorrhoea (understood as an early stage of what may or may not develop into a pox) with mercury.[15] In some cases, his provision of follow-up care reveals instances of lasting facial disfigurement. Mrs Turner is treated with salivation pills and her pox apparently cured: ‘onely’, Binns notes, ‘for want of care in the healinge of the ulceration of her goomes [gums] and cheekes there grewe some hard sicatrixe one the inside of her cheeks soe that hindard the openinge of her mouth wide. otherwayes wel praysed be god’ (f. 157v). It is unclear whether Binns blames the want of care on Mrs Turner for not following through on his suggestions for aftercare, his own regimen, or if another practitioner was involved in the ‘want of care’. If the scarring was restricted to the inside of her cheeks, Mrs Turner’s facial difference would not necessarily have been apparent until she wanted to move her mouth in a specific way, thus aligning her case with the concerns about movement raised by Bulwer.
Binns does explicitly acknowledge his own difficulties in the case of Jone Carter in May 1639. After a fluxing by a ‘Quacke’ three years ago that has resulted in persistent salivation Jone now ‘hath the lower mandible corrupt (& the teeth fallen forth)’ with swelling, ulceration and hardness across her chin and jaw. After ulceration caused scarring that prevented her from opening her mouth fully, the quack cut it, incidentally causing ‘a contraction of some branches of sinewes downe her necke, that she could nether open well her mouth nor lifte up her heade much’. While able to restore this movement, Binns’ treatment ultimately results in the exposure and disconnection of the entire mandible (the lower jaw bone), which by September is ‘lyinge loose in the cheekes’ and is removed in two parts ‘wth much payne & wth a good force’. Binns records that after over three years of severe pain and salivation, the healing of the gums brings relief, ‘& she verie well praysed be god, & noe greate blemish onely her chinne a little shrunke in’ (f. 170r). From accounts given by modern individuals without jaw bones, it can also be assumed that she might have had some functional impairments with breathing, speaking, eating and/or drinking (e.g. Warnke, et al, 2004).
In addition to scars from healed cuts, we can assume that many of Binns’ other patients carried scarring of some level after treatment, such as the man burnt by gunpowder in the face, hands and hair, at the Bear in Friday Street, even though Binns describes him as ‘well’ and closes his case only 12 days after the accident (f. 81r). Some of his venereal cases include ulceration and bone loss from the forehead that would be temporarily and then permanently disfiguring. In May 1633 he treats Mrs Lightfoote’s face with mercury and aqua fortis (‘strong water’; nitric acid), which would almost certainly have caused its own damage. Binns indeed records that ‘it caused paine but did noe good’ (f. 151r). A shoemaker, Mr Bottley, likewise loses ‘some peeces of bone oute at [his] gumme’ after shattering his jawbone falling from a horse, which may have caused some visible sinking of his cheek (f. 110v). Binns also records dissatisfaction at the result of his treatment for Mr Frances Tilney of Grays Inne, whom he treats for an apostem on the chin. Binns treats him in several stages with the caustic stone to open it into a wound and dispel the purulent matter. Binns’ disappointment with the aesthetics of the outcome is evident in his remark that the sore is healing after twenty days, ‘but the siccatrixe [scar] girte downe his chinne’ (f. 188r). Such qualified results, when combined with the risks inherent in any medical treatments, might have caused individuals with minor facial disfigurements some hesitation before seeking interventions from even respected hospital surgeons such as Binns.
Serious head wounds
https://dx.doi.org/10.15180/191111/007Where wounds of the face and head were judged to be life-threatening, surgeons’ first priority was to prevent death. If the patient did die, the surgeon might then be called in to testify about the nature of the wound in any criminal trial. Binns does not document any interactions with law enforcement, although some cases suggest the violence of the wounding might have raised the possibility of legal action. He records stitching a facial wound of the lutenist Mr Asberrie, after he brawled with a French lutenist called Gottier in Covent Garden on 10 May 1634, and therein ‘had a peece of his cheeke bitten out the breadthe of a yench & longer one the lefte side from the corner of his mouthe & nether lippe downe to the lower parte of his Jawe, & as muche tore up towards his cheek’. Binns stitched and dressed the wound, and appears to have been happy with the result, assessing the patient as ‘well ye 5t June’ (f. 207r). One also wonders whether there were any legal consequences following a case of 4 May 1641, wherein ‘One Mrs Grundis…by a blowe of her husbandes ffiste had the midle parte of the gristle of her nose broke’. Binns records treating her twelve hours after the injury, pushing it back into place ‘wth muche adoe & payne to her’ and applying ‘my Balsam’ (f. 207r).
In several cases, facial wounds are left with minimal intervention until further symptoms suggest internal injuries. At this point, Binns understandably prioritises symptoms such as vomiting and bleeding over concern for exacerbating disfigurements, although his reports are scant enough that we can’t know exactly what precautions he might have been taking in his method. Woodall similarly advised that surgeons not be too hasty to use trepanation (one of Binns’ rare cases is included below), estimating that only one in ten cranial fractures actually required it, and in such life-threatening cases the location was to be guided solely by the fracture itself (Woodall, 1655, sig. D3r).
Binns’ restraint and changing priorities between face and brain injuries are demonstrated across numerous cases. On 11 September 1635, a serving woman in a boat on the Thames is struck on the right side of the forehead by a stick thrown from another boat, and ‘by ye Blowe ye bone was layed bare the breadth of a shillinge’. Binns does not record any treatment at this point, suggesting that either the woman did not seek assistance from him then (though she might have applied bandages, etc, at home) or it was so minimal that he did not think it worth recording. He notes that ‘She was well & farr from any symptoms till ye 23 of September’ when she began to vomit and show a ‘quotidian intermitting fever’, suggesting more significant injuries. The wound is therefore ‘layde further open’ to check for a fracture, which is not found, but would of course lead to more significant scarring if the woman survived. On 30 September they trepan, releasing ‘greate quantity of purulent matter betwixt Cranium & dura mater very stinking’, and apply ‘oyle of Roses upon ye brayne’, but she dies on the ‘1st or 2d October’ (f. 7v). Woodall also recommends oil of roses for wounds of the head, along with rose-infused honey (1655, sig. K1v). In a case from 1638, a forehead wound resulting from a drunken scuffle and thrown pot is attended to as a possible skull fracture and trepanned, after the patient’s servant testifies that the patient’s vomiting is highly unusual – ‘he never used to vomitt though he had drank never soe much soe it was likely by reason of his wounde’ (f. 166r). Similarly in December 1647 a man ‘received a blowe (wth a pinte pott flunge at him) upon the side of the Temporal Muselle’ which created a ‘wounde downwarde the breadth of 2 fingers [and] lefte the cranium bare wth a fissure’. Binns ‘drest it up wth warme balme’ and ‘soft dosells’ (i.e. dossils, a lint or rag) allowing the area around the wound to swell. The man remained in bed, or at least in his room, and the wound appeared to be healing well until the sixth day, ‘then he came downe stayres & drinking stronge beere he was much distempered & could not sleepe’. Binns therefore bled him and administered a clyster (enema) and another poultice to the wound, and it began to heal more rapidly. Binns did not describe the patient as ‘well’ until forty-two days after the accident, indicating reluctance to dismiss the case too early in case of another relapse (f. 16v).
Binns’ cautious privileging of symptoms such as vomiting as signs of serious internal injury over his customary non-intervention and the application of scar-preventing aesthetic remedies to facial wounds is especially evident in his record of a case from another surgeon. A barber named William received a knife wound to the temple in December 1636, and his surgeon initially restricted his treatments to ‘pledget & a plaster’, even after William started vomiting blood. The patient became ‘somewhat stupid then came to him selfe but complained of greate payne in the wounde & for as he could not sleep in the night & soe continued till ye 9 or 10th daye then Harvey his surgeon gave him a purge but afore then had neither given him Clyster nor opened vayne nor applied any thinge to his wounde more than pledget & a plaster wch did not worcke but made him very sick’. It’s at this point that Harvey administers a purgative, but we are told that ‘all that side was paralitick one wth ye wounde was & he in a delirium & next daye he dyed’ (f. 7v). Binns’ record of this case, which conveys a sense of surprise at Harvey’s choice of limited regime, suggests that in this case he did not agree with his colleague’s restraint, and largely blamed him for the poor outcome. Despite his own generally cautious approach, Binns expresses clear disapproval of this overly restrained treatment of a facial wound.
Conclusion
https://dx.doi.org/10.15180/191111/008Theoretical principles set out in textbook discussions and lectures by practitioners like Alexander Read, John Woodall and Daniel Turner identified a wide range of techniques and alternative practices that surgeons could use to minimise visible damage to patients’ faces caused by accidents, disease, or even their own treatments. The unpublished case notes of surgeons like Joseph Binns are useful for showing that elements of these principles were indeed put into practice, illustrating, for example, the use of the dry seam, early removal of stitches, or reduction in their use.
Sources like Binns’ case notes can also provide us with a greater awareness of the number of people living with different forms of facial disfigurements in the early modern period, and can contribute to our understanding of expectations about the role of medicine in personal appearance. Disfigurements might predate these individuals’ engagements with the surgeon by some time and be self-treated or simply borne by the individual until further discomfort prompted them to seek intervention. In some cases disfigurement could follow an encounter with the surgeon, as cuts and medications left further marks on the skin. Several of Binns’ patients were left with scars from the wound, the disease, or the treatment itself. Surgeons were aware of these limitations, and especially their own potential to exacerbate aesthetic problems. Public and practitioner awareness of the limitations of surgery may have impacted not only the outcomes, but also the initial expectations and impetus for individuals with facial marks, injuries or other conditions to seek out medical interventions, as well as their experiences of living with facial difference in themselves and others.
There is plenty of evidence in the medical sources for practitioners’ appreciation of the functionalist aspects of the face, such as its importance for eating, drinking, breathing, speech, and facial expression, and resulting desire to preserve facial movement and form. There is an unsurprising prioritising of head wounds whenever the life of the patient was at risk, including the opening up or infliction of wounds in procedures like trepanning to release fluid and pressure on the brain. Alongside this, however, we see appreciation for the aesthetics of the face and its importance for personal beauty and identity, and the impact of such philosophy on prescriptions for ideal practice within surgical manuals. Binns’ case notes then demonstrate the nuanced application of these principles in everyday hospital medicine. As with the twenty-first-century practices discussed by McCaul, early modern facial surgery blended necessity with aesthetic concern on the understanding that this was a uniquely vulnerable, exposed and identifying part of the body, and that facial operations were therefore laden with ‘an additional burden of significance and responsibility’. A patient with a facial wound might be judged ‘well’ and dismissed at the point that their wound began to form a scar, but early modern surgeons like Binns were keen to ensure that these ‘ill favoured scarres’ and the resulting facial difference were as small as possible.
Tags
Footnotes
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text
Back to text